Understanding VATS Thymectomy Surgery: A Comprehensive Guide

When it comes to treating thymic tumors, myasthenia gravis, and other diseases of the thymus gland, VATS thymectomy surgery has emerged as a revolutionary technique. This minimally invasive procedure offers numerous benefits over traditional open surgery, including reduced recovery times, less postoperative pain, and smaller scars. In this article, we will delve deeply into the details of VATS thymectomy surgery, discussing its indications, procedure, advantages, recovery process, and frequently asked questions.
1. What is VATS Thymectomy Surgery?
VATS, or Video-Assisted Thoracoscopic Surgery, is a minimally invasive surgical technique used to access the chest cavity through small incisions, guided by a camera and specialized instruments. During a VATS thymectomy, surgeons remove the thymus gland, which plays a crucial role in the immune system, particularly during childhood.
2. Indications for VATS Thymectomy
VATS thymectomy is indicated for various conditions, including:
- Myasthenia Gravis: An autoimmune disorder that affects nerve impulses and muscle contractions.
- Thymoma: A tumor originating from the thymus gland, which may or may not be benign.
- Thymic Carcinoma: A rare and aggressive form of cancer affecting the thymus.
- Other Thymic Disorders: Conditions that affect the structure or function of the thymus gland.
3. Benefits of VATS Thymectomy Surgery
The advantages of opting for VATS thymectomy surgery over traditional open surgery include:
- Minimally Invasive: Smaller incisions lead to less trauma to the body.
- Reduced Pain: Patients typically experience less postoperative pain than with open surgeries.
- Shorter Hospital Stay: Many patients are able to go home within a day or two following the procedure.
- Faster Recovery: The minimally invasive nature of the surgery often results in quicker recovery and resumption of normal activities.
- Cosmetic Benefits: Smaller incisions result in less noticeable scars.
4. The VATS Thymectomy Procedure: Step-by-Step
Understanding the VATS thymectomy surgical process can help alleviate concerns for prospective patients. Here’s a comprehensive step-by-step guide to the procedure:
4.1 Preoperative Preparation
Before undergoing surgery, patients will have a thorough evaluation, including imaging studies and laboratory tests. It is essential to discuss any medications and health conditions with the surgical team.
4.2 Anesthesia
Patients are given general anesthesia to ensure they are unconscious during the procedure, allowing for a pain-free experience.
4.3 Surgical Technique
The surgeon performs the following steps:
- Incisions: Small incisions (usually 3-4) are made on the chest wall.
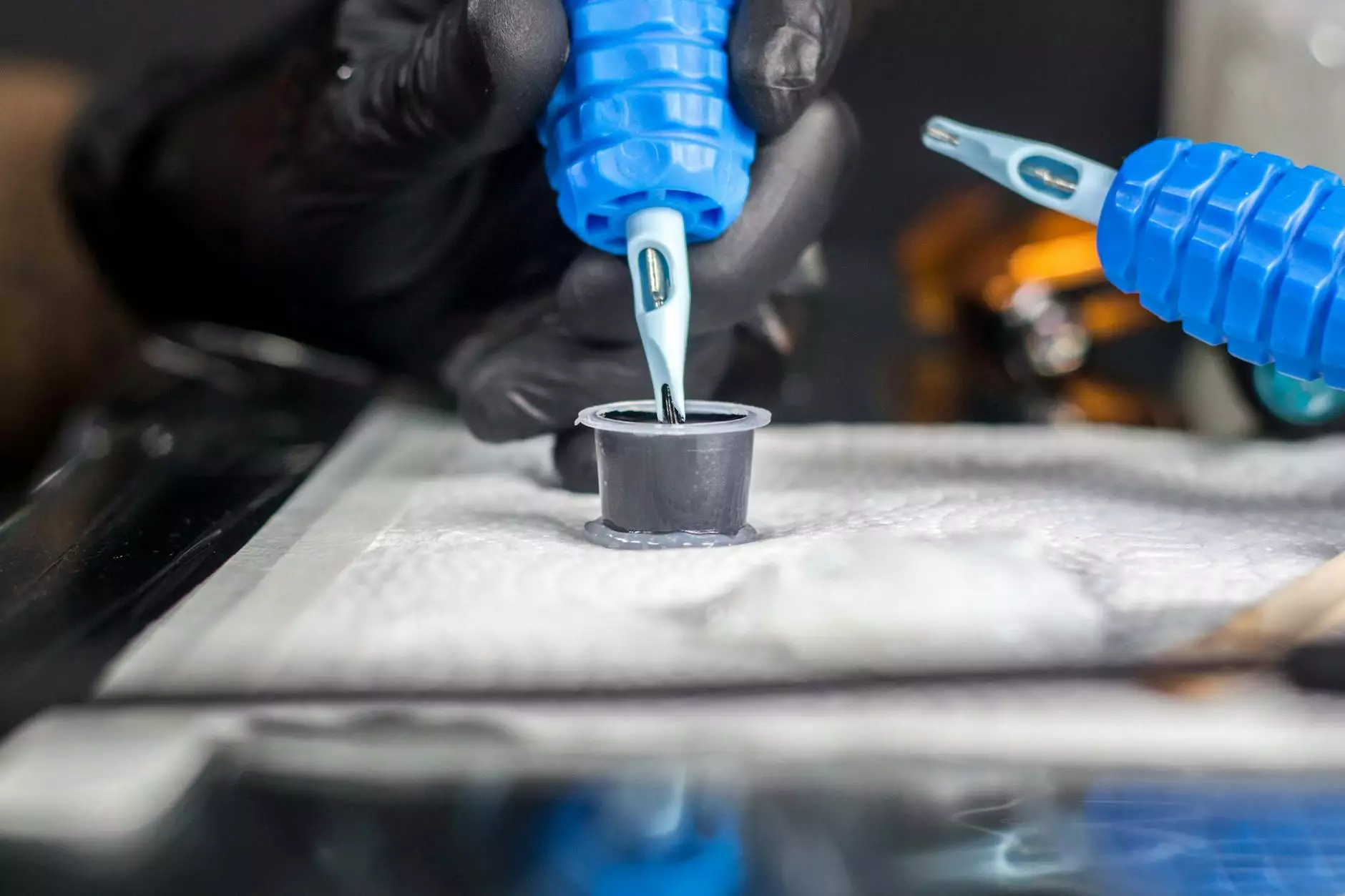
- Inserting the Camera: A thoracoscope, equipped with a camera, is inserted through one incision, providing the surgeon with a view inside the thoracic cavity.
- Instrument Manipulation: Specialized instruments are inserted through the additional incisions.
- Thymus Removal: The thymus gland is carefully dissected and removed. If a tumor is present, it's also excised.
- Closure: The incisions are closed, usually with sutures or adhesive strips, and the patient is moved to recovery.
5. Recovery After VATS Thymectomy Surgery
Postoperative recovery is a crucial stage of the VATS thymectomy surgery journey. Here’s what to expect:
5.1 Immediate Recovery
After the surgery, patients are monitored in a recovery room for any complications related to anesthesia or the procedure. Pain management will begin immediately.
5.2 Hospital Discharge
Most patients can expect to be discharged within 24 to 48 hours, depending on their overall health and recovery progress. Prior to discharge, a physician will provide detailed instructions on wound care and pain management.
5.3 At-Home Recovery
Once home, patients will need to take care during recovery. Typically, recovery may take several weeks, during which patients are advised to:
- Limit physical activity, especially heavy lifting.
- Attend follow-up appointments to monitor healing.
- Report any unusual symptoms, such as fever or excessive pain, to their healthcare provider.
6. Potential Risks and Complications
As with any surgical procedure, there are risks involved with VATS thymectomy surgery. While complications are rare, they may include:
- Infection: While the use of minimally invasive techniques reduces the risk, infections can still occur.
- Bleeding: Excessive bleeding may require a transfusion or further intervention.
- Damage to Surrounding Structures: There is a risk of inadvertent damage to surrounding organs.
- Respiratory Issues: Some patients may experience temporary respiratory complications post-surgery.
7. Conclusion
VATS thymectomy surgery represents a remarkable advancement in surgical oncology and treatment for autoimmune disorders. With its numerous benefits and minimal invasiveness, it is reshaping the standards of care for patients with thymus-related conditions. If you or a loved one are considering this procedure, we encourage you to consult with a specialized surgeon to discuss your options and what’s best for your health.
8. Frequently Asked Questions (FAQs)
8.1 How long does the VATS thymectomy surgery take?
The duration of the surgery typically ranges from 2 to 4 hours, depending on the complexity of the case.
8.2 Will I need follow-up treatment after surgery?
Depending on the diagnosis, follow-up care may be necessary, including regular check-ups and possibly medication.
8.3 Are there alternatives to VATS thymectomy?
Alternatives such as open thymectomy or medical management may exist but should be discussed with your healthcare provider.
For more information about VATS thymectomy surgery and related treatments, visit neumarksurgery.com.